MSM (Methylsulfonylmethane): The Missed Nutrient for Building Mucosa, Permanent SIBO/SIFO Recovery, and Boosting Neurological Function
If you’ve ever found yourself reacting to foods that once felt safe, feeling confused why “clean eating” still isn’t working, or sensing your gut lining feels fragile no matter how careful you are…you are not alone.
Many of today’s chronic gut-immune clients aren’t struggling because their bodies are broken. They’re struggling because the terrain has been depleted faster than it can rebuild.
And one of the most overlooked nutrients in that terrain? Bioavailable sulfur. Specifically in the form of MSM.
Sulfur sits at the crossroads of:
Mucosal barrier strength
Collagen repair
Detoxification and glutathione production
Nervous system regulation
Microbiome balance and motility
Histamine stability
Yet most people today are sulfur-depleted despite being on nutrient-dense diets.
Why The Mucosal Lining Matters
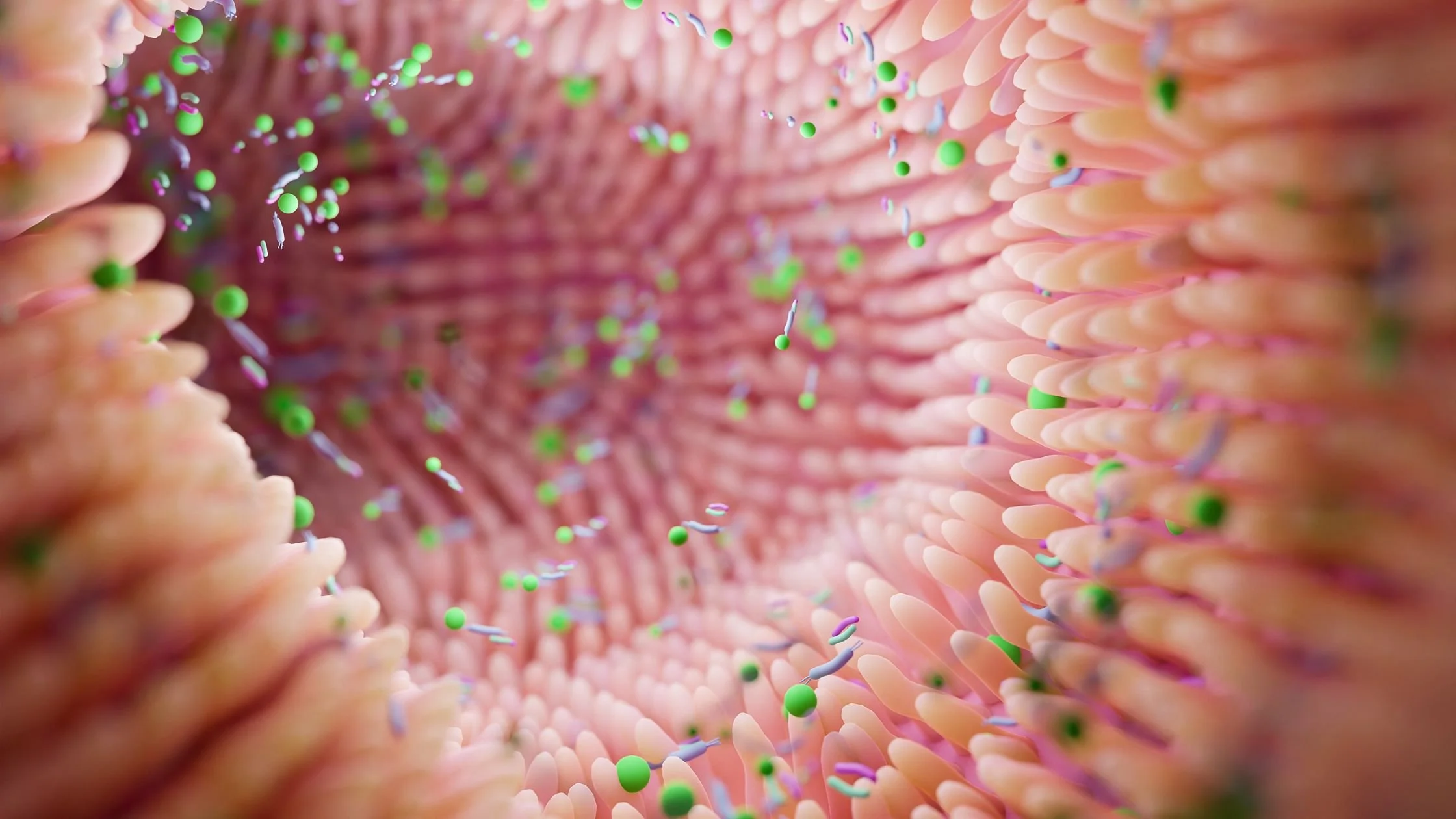
Your gut lining is like an ancient castle wall supported by a protective moat. This castle is very spectacular and has redundant yet diverse defense systems to keep it safe. One protection is a moat.
The mucosal lining is the moat around the castle. The castle walls (your epithelial lining + villi) can only stay strong when the moat is full and healthy.
You also have on guard the secretoryIGA deciding what enters circulation and what stays out. These immune peacekeepers are sorting friend from foe so that your immune system doesn’t over react. If the defense structures of the castle aren't fully functional, the secretoryIGA patrollers work much harder.
The goblet cells of the intestines create something called mucin which is the mucosal lining protecting your intestines from undigested food, enzymes, and bacteria. Most people think mucus is bad, especially when we are congested in the sinuses, but your body sees mucus as a protective barrier and is greatly desired by your intestinal cells.
When the mucosal lining thins, you experience:
Food sensitivities
Histamine flares
Constipation or loose stools
Fatigue and post-exertional crashes
Skin flares
Reactivity to supplements
Heightened nervous system responses
Most people are told this is “inflammation.” But inflammation is often downstream of mucin depletion, sulfur deficiency, and microbial imbalance.
Your Mucosal Lining Barrier Includes:
A layer of mucus (produced by goblet cells)
A network of immune cells underneath (GALT)
The epithelial cell layer (tight junctions, villi, etc.)
The Dominant Theory: “Mucus-Eating” or “Mucin-Degrading” Opportunists become “Pseudo-Pathogenic”
There is a beautiful synergistic relationship between the mucosal lining and the bacteria in your gut. The bacteria in your gut nourish the intestinal lining and mucosa while also the mucosal lining can be a great food source in times of need for specific bacteria.
This is not a bad thing, it is an essential redundancy found in the body because of the importance of beneficial bacteria in our immune and overall health.
The main thing I see in my clients with persistent fatigue, lingering bloating and GI symptoms, autoimmunity, chronic reactivity, collagen disorders, and histamine issues is the common theme of leaky gut and inflammation stemming from nutrient deficiencies simultaneously with bacterial deficiencies/overgrowths.
This is crucial to understand that it is a two-way street both bacteria and nutrient deficiencies lead to poor intestinal cell structure and mucosal collapse.
From the Bacteria Point of View:
Healthy gut microbes like Akkermansia muciniphila and Bifidobacterium bifidum gently “graze” the mucus layer, stimulating renewal.
But if dietary fiber and polyphenols are too low, or if keystone species are lost, opportunistic or pseudo-pathogenic microbes begin over-consuming mucin for energy.
This leads to mucosal thinning, permeability, and immune activation… the root of “leaky gut” and chronic inflammation.
Because every gut is unique, it’s almost impossible to predict when microbes will shift from balanced grazing to mucin over-consumption. This is what leads me to look at the mucin-degrading bacteria problem from a different angle.
“The challenge is, it is very bio-individual and near impossible to determine exactly how long it will take without feeding these microbes, for them to begin over-consuming the mucin. ”
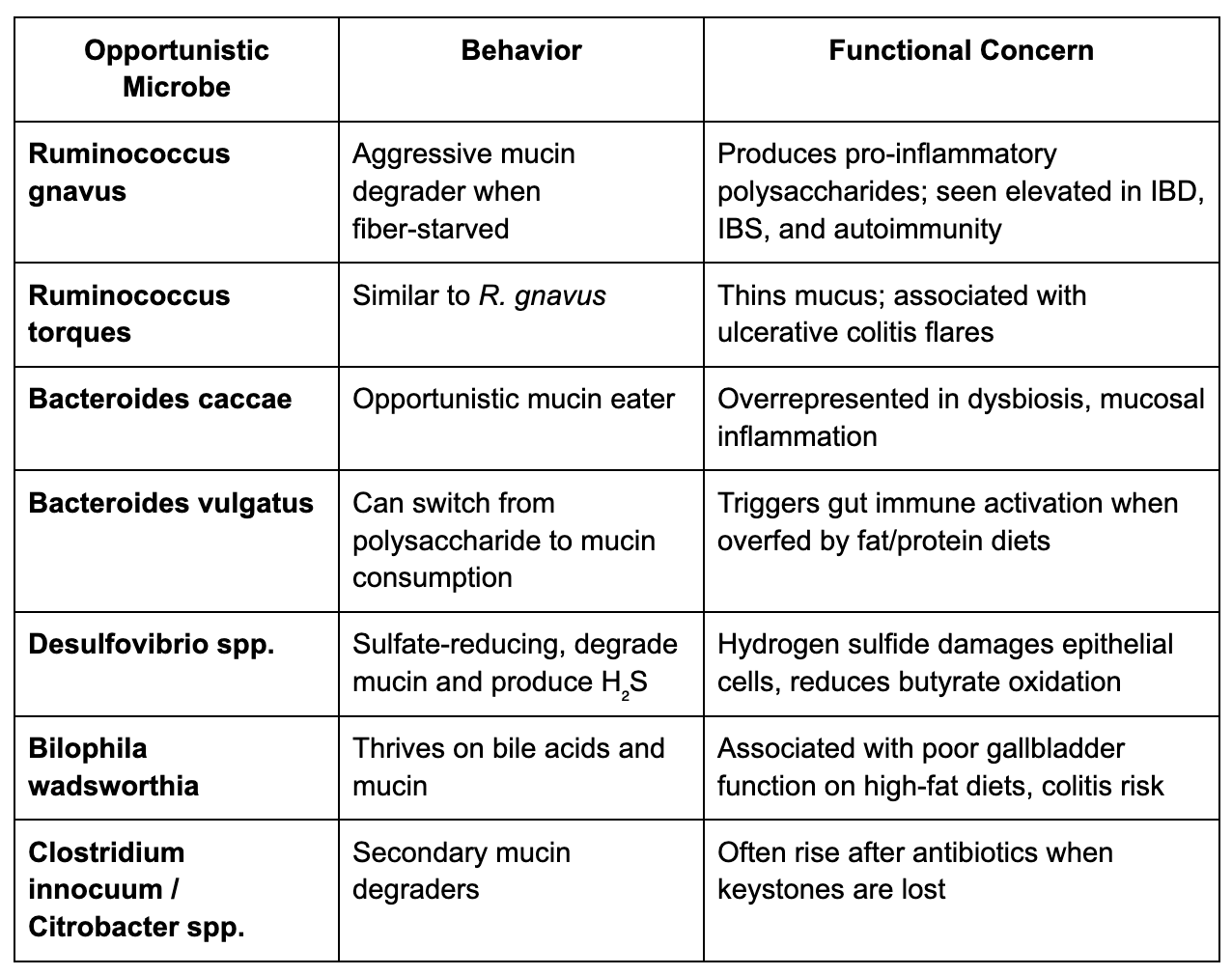
Here is a list of the species that can opportunistically degrade mucosa:
The typical fiber-starvation pattern in the gut looks like:
Low Akkermansia muciniphila and Bifidobacterium bifidum
High Ruminococcus gnavus or Bacteroides vulgatus
High H₂S hydrogen sulfide production/ SRB bacteria (ex: Desulfovibrio, Bilophila)
Low SCFA function (especially butyrate, can be seen in the BiomeFX lab)
From the Nutrient-Deficiency Point of View:
What is Mucin Made of?
Mucosal Barrier = Sulfur-Rich Structure
Your intestinal mucosal layer is composed primarily of mucins, large glycoproteins (glyconutrient + amino-acid) secreted by goblet cells. Each mucin molecule has two critical features:
Carbohydrate side chains (rich in the healing glyconutrient sugars: fucose, galactose, N-acetylglucosamine, sialic acid)
Sulfated residues; the “sulfomucins”
The sulfate groups (-SO₃⁻) are essential because they:
Give mucin its negative charge, allowing it to form a slippery, hydrated gel barrier
Protect mucin from bacterial enzymatic degradation
Bind cations and toxins for elimination
Regulate microbial attachment (so only beneficial bacteria like Akkermansia can gently graze on it)
So, sulfur deficiency can weaken mucin structure and resilience.
Some practitioners, myself included, observe that when the body becomes sulfur-deficient, the rise in sulfate reducing bacteria (SRB) and mucin-degrading bacteria may actually be a compensatory response.
In other words, the microbiome may be trying to liberate sulfur from mucin to help us; not harm us, even though the process ends up thinning the mucosal lining and worsening symptoms over time.
It’s a bit like parts-work in IFS: our internal parts often step in with protective strategies that originally evolve to help us, but when those strategies persist without support or regulation, they can unintentionally contribute to the very problem they were trying to solve.
“ In other words, the microbiome may be trying to liberate sulfur from mucin to help us; not harm us, even though the process ends up thinning the mucosal lining and worsening symptoms over time.”
Key Takeaway: Your Mucosal Lining Barrier is not only influenced by mucin-eating bacteria and presence of birth microbes, it is also influenced by your body’s nutrient deficiencies, such as sulfur.
Why MSM Before Probiotics
Many people are told to seed probiotics and feed with prebiotics and fiber…
Yet when the mucosal layer is thin, even beneficial bacteria can produce pro-inflammatory byproducts and affect the gut lining, especially if there is a thin mucosal barrier.
In fact, supplementing and trying to seed with probiotics and prebiotic fiber before building the mucosal lining may lead to immune activation as cited in this research article, “The mucus layer lining the colonic epithelium is the first line of defense limiting exposure of epithelial cells to ingested food components, digestive enzymes, and microorganisms.”
Nothing is either ALL-bad or ALL-good. Everything in this complex system of our body plays a role and there is redundancy and diversity of complex processes (bacteria feeding mucin, and mucin nourishing bacteria) within the complex system.
However, this often explains why clients say:
“Probiotics make me worse”
“Fiber hurts my stomach”
“I react to everything right now”
So if the terrain is fragile and stimulation makes you worse, what do we do instead?
We rebuild the biochemical scaffolding first.
Why Sulfur Deficiency Is So Common Now
We’re seeing a modern sulfur gap. Even with nutrient-dense ancestral diets rich in sulfur-containing amino acids such as methionine and cysteine, many people still are not rebuilding their mucosal lining the way we would expect.
Years ago, a properly constructed ancestral diet often repleted sulfur. Today, more clients need a targeted high dose of MSM to overcome environmental toxicity (e.g., glyphosate) and finally tolerate more foods.
In clinical practice, we are consistently seeing more individuals who stall despite excellent diets. This suggests that food alone is not enough anymore to restore sulfur status in today’s environment.
Glyphosate, mineral depletion, and microbial shifts mean many people can’t efficiently convert sulfur-containing foods into usable sulfate.
MSM directly supplies safely tolerated sulfur, which your body uses to build glutathione (detox), synthesize collagen (repair), and give structure to the gut’s mucosal lining.
What sulfur does (and why you feel it):
Without dietary sulfur we would die: This is an essential nutrient that you can’t easily test for deficiency status but with the presence of glyphosate building over the last 40 years, research shows that everyone in the United States has been exposed.
Mucosal lining: Sulfur supports the elasticity and integrity of mucus. Better mucosa leads to fewer random reactions.
Collagen, hair/skin/nails: Collagen fibers are linked by sulfur bonds; MSM often improves skin tone, texture, and hair quality as stores rebuild.
Joints & aches: Clients frequently notice less joint pain as sulfur status rises. Especially when they also reduce high-glyphosate foods (like conventional oats/chickpeas/gluten/barley/corn).
Detox capacity: MSM is a key building block for glutathione, your master antioxidant.
The Science of Glyphosate and Sulfur Deficiency:
Glyphosate's core biochemical mechanism is to block an enzyme route of bacteria, fungi and plants which negatively impacts keystone birth-microbes like Bifidobacterium, Lactobacillus, and Faecalibacterium.
Then more resistant opportunistic species like proteobacteria and sulfate reducing bacteria (SRB) become overgrown. This shifts the microbiome towards sulfate reducing bacteria dominance which has the byproduct of hydrogen sulfide, a common form of SIBO/bloating.
When in balance hydrogen sulfide helps regulate mucin turnover but in excess it becomes toxic to the lining of the colon cells. This alone can negatively affect the mucosal lining.
But there is another reason that is critical for choosing MSM with glyconutrients first to build our mucosa. When glyphosate reduces our “good” bacteria, the body shifts toward sulfite accumulation (which is more toxic to our body and requires molybdenum to be turned into sulfate). With molybdenum functionally deficient and Glyphosate also chelating minerals such as manganese, iron, cobalt, magnesium and zinc we become sulfur deficient and sulfite toxic. Clinically this looks like sulfite sensitivity, impaired detoxification, and chronic symptoms.
Not only this, but glyphosate mimics systemic sulfur deficiency even when dietary sulfur is adequate because it can interfere with all sulfation reactions in the body including mucin sulfation, detoxification of neurotransmitters, and hormone metabolism.
We use MSM to supplement for this sulfur deficiency because other sulfur compounds like sulfate salts, cysteine/methionine, plant sulfurs, and NAC can feed SRB overgrowth or may transiently raise hydrogen sulfide.
MSM bypasses this bottleneck and supplies sulfur in a safe, highly multifunctional and bioavailable way, without feeding sulfate-reducing bacteria.
This is why clients often report:
Stronger mucosa
Improved tolerance for foods
Less joint and nerve pain
Increased motility
Calmer histamine responses
Emotional steadiness and nervous-system calm
Which Comes First The Chicken Or the Egg
We often ask, “Which comes first? Is it the microbiome imbalance or the mucosal collapse?”
The truth is, it’s rarely one or the other. It’s a feedback loop.
When sulfur is low, oxidative stress rises, detox slows, mucosal sulfation weakens, and the lining thins. At the same time, keystone microbes lose fuel, and opportunistic species step in, trying to compensate. The body and microbiome are both doing their best to help, only with limited resources.
This is why foundational nutrient rebuilding matters. We don’t pick sides between “bugs first” or “nutrients first.” We strengthen structure, replenish sulfur and glyconutrients, and calm stress physiology so the system can reorganize into balance.
When we do this, the body stops reacting and starts trusting again. Digestion stabilizes, bacteria shift from survival mode into symbiosis, and food freedom returns.
Foods & Nutrients That Build the Mucosal Lining
Key Nutrients that Build Mucosal Lining
Food Sources To Build Mucosal Lining
Interestingly many of the foods highest in the nutrients that build the mucosal lining are ancestrally consistent foods.
Action: The Rooted Resilience Method for Rebuilding the Mucosa
At Nutrition with Confidence, the Rooted Resilience Method approaches mucosal repair as a systems-based individualized process. When the mucosal barrier collapses, whether from lifestyle, microbial imbalance or nutrient depletion, the goal isn’t just to patch it up; it’s to rebuild it using small and slow solutions that beautifully and creatively spark deep lasting transformation even in the marginal unintended places of our body-mind-and-soul.
1. Rebuild the Structural Matrix
We begin by replenishing the body’s collagen-building foundational nutrients of mucosal integrity.
A high-dose MSM protocol provides bioavailable sulfur, fueling the synthesis of collagen, mucin, and glutathione.
Glyconutrients (specialized plant sugars) are added to support cellular communication, epithelial regeneration, and immune balance within the gut lining.
2. Fortify the Immune Barrier
If stool data or symptoms suggest pathogenic overgrowth or immune stress, we then bring in immunoglobulin support.
Serum-derived immunoglobulins act like natural binders. These neutralize bacterial toxins and stabilize the gut ecosystem.
When needed, we layer in HU58®, a resilient Bacillus subtilis probiotic strain that gives off natural antibiotics to rebalance the microbial ecosystem and reduce opportunistic load.
3. Assess and Personalize with Testing
Once the foundational layers are in place, we use BiomeFx® stool testing to map out the unique microbial terrain. We prefer this test because it not only highlights which keystone species are missing and which mucin-degraders may be overactive, but it also measures overall function in the larger picture of the microbiome.
Here is a case of how function helped prioritize next steps: this client’s stool test showed his microbiome was trending toward a sulfate-reducing, proteolytic environment, but the H₂S marker itself was not alarming and his overall diversity and function showed there was balance with butyrate production.
His acetate and propionate were low, but the utilizers of resistant starch (like Ruminococcus bromii and Roseburia intestinalis) were absent.
Without those keystone species, resistant starch can ferment improperly, feeding Proteobacteria and worsening gas, ammonia, or polyamines.
This data-driven snapshot allowed us to refine this client’s plan to wait until symptoms stabilized and stool regularity improved before introducing Resistant starch like green banana flour.
Testing can be done either before or after the initial mucosal rebuild phase, depending on symptom severity, cost aversion, and readiness.
4. Reseed and Feed the Ecosystem
With a cleaner, stronger foundation, we then reseed the gut with targeted probiotic strains and prebiotic fibers chosen specifically for your microbiome profile.
The goal: restore diversity, rebuild keystone species like Akkermansia and Bifidobacterium, and reinforce mucosal resilience for the long term.
Who should go extra-slow:
Histamine-reactive clients, those with sensitive skin, or anyone who’s highly reactive to new supplements. MSM helps stabilize, but dose matters.
Safety & practical notes:
MSM is generally well tolerated; start low and slow.
Transient reactions usually reflect mobilization/detox not an allergy. Adjust pace; don’t power through severe symptoms.
As with any protocol change, coordinate with your provider especially if you’re on prescription meds or navigating active flares.
Bottom line:
MSM often acts as the missing key nutrient for restoring essential sulfur to the body, and the gut’s mucosa, collagen repair, detox capacity, and stabilizing histamines (stay tuned for our next blog on how sulfur impacts histamines), making it easier to expand foods and feel human again.
You’re not broken - your mucosal lining is.
You’ve already done the hard work, tried animal-based eating, eliminated trigger foods, and cleaned up your lifestyle. But you’re still stuck. The fatigue, food reactions, and pain haven’t fully resolved, and your gut feels fragile no matter what you eat.
The Mucosa Building 3-Month Guide was created for people like you who’ve hit a plateau in their healing after endless diets and protocols. This guided self-paced course walks you through the same foundational process I use with clients in my practice to rebuild the gut’s mucosal barrier, restore immune balance, and calm systemic inflammation.
Inside, you’ll learn how to safely and effectively use my High-Dose MSM Protocol and Glyconutrient Repair System…two of the most powerful tools for rebuilding the gut mucosal lining, collagen structure, and nervous system tolerance.
It’s simple, it’s beautiful.
You’ll get clear guidance for every sensitivity level, from delicate to strong responders, plus troubleshooting support for detox symptoms and pacing your increases with confidence.
This protocol guide is ideal if you experience:
Persistent bloating, IBS, SIBO, or SIFO that hasn’t resolved
Food reactivity or histamine intolerance that keeps expanding
Collagen disorders, joint or connective tissue pain
Sulfur intolerance or chronic detox sensitivity
Post-animal-based diet stagnation or plateaued healing
Over 12 weeks, you’ll be guided step-by-step to rebuild your mucosal barrier, strengthen collagen integrity, and calm inflammation at the root. You’ll learn how to nourish your gut instead of restrict it—and discover that resilience is something you can rebuild.